Hysteroscopic Adhesiolysis: A Minimally Invasive Treatment for Asherman’s Syndrome
Asherman’s Syndrome is a condition characterised by the occurrence of intrauterine adhesions, also known as uterine synechiae. These adhesions can form because of uterine trauma, such as previous surgeries, infections, or endometrial damage. Asherman’s Syndrome can lead to various reproductive health issues, including menstrual abnormalities, infertility, and recurrent pregnancy loss. Fortunately, advancements in medical technology have paved the way for a minimally invasive treatment known as hysteroscopic adhesiolysis, which offers hope to women struggling with this conditio n.
n.
Asherman’s Syndrome can significantly impact a woman’s reproductive health, leading to distres
sing symptoms and difficulties when conceiving. However, with the advent of hysteroscopic adhesiolysis, a minimally invasive treatment, there is renewed hope for patients suffering from this condition. This article explores the various aspects of hysteroscopic adhesiolysis as a successful intervention for Asherman’s Syndrome.
Understanding Asherman’s Syndrome
Definition and causes
Asherman’s Syndrome, also known as intrauterine adhesions or uterine synechiae, refers to the formation of scar tissue within the uterine cavity. This scarring occurs due to trauma or damage t
o the endometrium, often resulting from previous uterine surgeries, infections, or postpartum complications. The adhesions can vary in severity, ranging from thin filmy bands to dense adhesions that completely obliterate the uterine cavity.
Symptoms and diagnosis
Women with Asherman’s Syndrome may experience menstrual abnormalities, such as decreased or absent periods, as well as pelvic pain and infertility. Diagnosing Asherman’s Syndrome typically involves a thorough medical history review, physical examination, and imaging techniques like hysterosalpingography or sonohysterography.
Hysteroscopy, a minimally invasive procedure, is considered the gold standard for both diagnosis and treatment of Asherman’s Syndrome.
Conventional Treatment Options
When it comes to managing Asherman’s Syndrome, the treatment approach depends on the severity of the adhesions and the symptoms experienced by the patient. Conventional treatment options include hormonal therapy and surgical intervention.
Hormonal therapy
Hormonal therapy aims to promote the regeneration of the endometrium and prevent further adhesion formation. It typically involves the administration of oestrogen and progesterone to stimulate the growth of the uterine lining. While hormonal therapy may be effective for mild cases, it is often insufficient for significant adhesions.
Surgical intervention
In more severe cases of Asherman’s Syndrome, surgical intervention is often required to remove the adhesions and restore the normal uterine cavity. Traditionally, the surgical approach involved dilation and curettage (D&C) or transcervical resection of adhesions (TCRA). However, these procedures have limitations and may not be as effective in removing extensive adhesions.
Introduction to Hysteroscopic Adhesiolysis
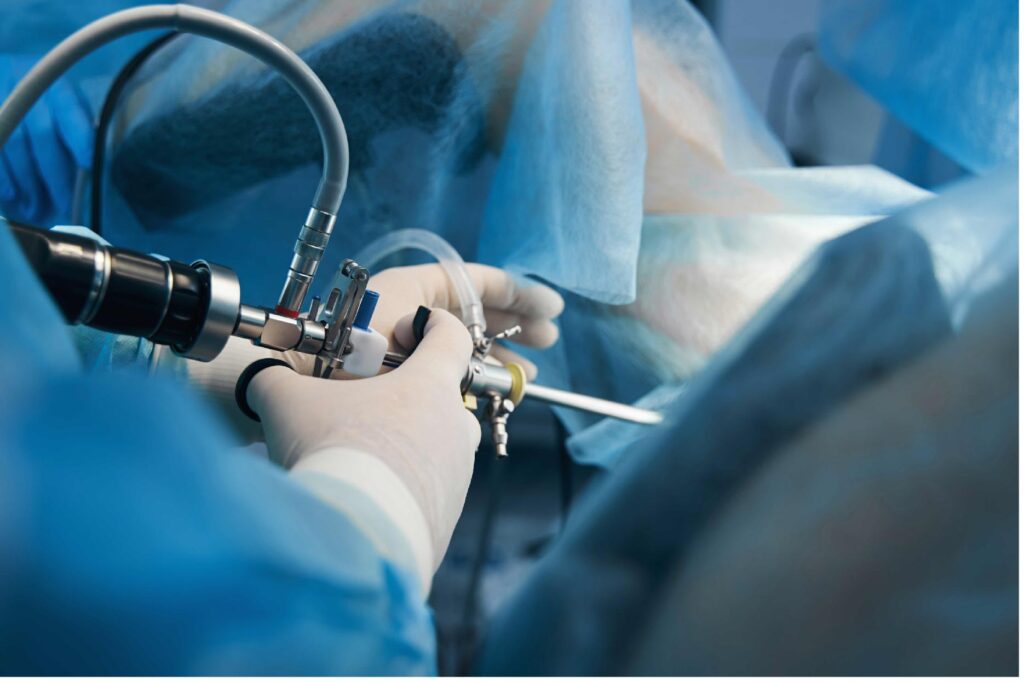
Definition and procedure overview
Hysteroscopic adhesiolysis is a minimally invasive surgical procedure performed using a hysteroscope, a thin and flexible instrument that allows direct visualisation of the uterine cavity. The procedure aims to meticulously remove the intrauterine adhesions, restoring the normal anatomy and functionality of the uterus.
Benefits of hysteroscopic adhesiolysis
Hysteroscopic adhesiolysis offers several advantages over traditional surgical techniques. Firstly, it is a minimally invasive procedure that can be performed on an outpatient basis, minimising hospital stays and promoting faster recovery.
Secondly, hysteroscopy allows for precise identification and removal of adhesions, ensuring optimal results. Additionally, the procedure provides a clear view of the uterine cavity, facilitating the evaluation of other potential abnormalities.
Preparation and Procedure
Before undergoing hysteroscopic adhesiolysis, patients undergo a thorough preoperative evaluation to assess their overall health and determine the extent of adhesions. The procedure is typically performed under general anaesthesia, although local anaesthesia may be used in certain cases.
Hysteroscopic equipment and techniques
During the procedure, a hysteroscope is inserted into the uterus through the vagina and cervix. The hysteroscope is equipped with a light source and a camera, allowing the surgeon to visualise the uterine cavity on a monitor. Specialised instruments, such as scissors, graspers, or laser devices, are used to remove the adhesions under direct visualisation.
Hysteroscopic Adhesiolysis Process
Insertion of hysteroscope
Once the patient is under anaesthesia, the hysteroscope is gently inserted into the uterus through the cervix. A sterile fluid, usually saline, is infused into the uterine cavity to expand it and provide a clear view.
Identification and removal of adhesions
Using the hysteroscope, the surgeon carefully examines the uterine cavity to identify the location, extent, and type of adhesions. The adhesions are then meticulously dissected and removed, layer by layer, using specialised instruments.
Techniques for adhesion separation
Different techniques may be implemented to separate adhesions during hysteroscopic adhesiolysis. These techniques include sharp dissection with scissors or electrosurgical instruments, mechanical separation with hysteroscopic graspers, or the use of laser energy to vaporise the adhesions.
Recovery and Follow-up
Postoperative care
Following hysteroscopic adhesiolysis, patients are typically monitored for a short period in the recovery area before being discharged. They may experience mild cramping and vaginal spotting for a few days. Pain medication and antibiotics may be prescribed to manage discomfort and prevent infection. Patients are advised to refrain from sexual intercourse and strenuous activities for a few weeks to allow the uterus to heal.
Potential complications and risks
While hysteroscopic adhesiolysis is considered a safe procedure, there are potential risks associated with any surgical intervention. These risks include infection, bleeding, injury to the uterus or other pelvic structures, and anaesthesia-related complications. However, serious complications are rare.
Monitoring and follow-up visits
Patients are typically scheduled for follow-up visits to monitor their recovery and assess the success of the procedure. Additional hysteroscopy may be performed to ensure that the adhesions do not recur. Depending on the patient’s specific situation, further treatment, such as hormonal therapy, may be recommended to support endometrial regeneration.
Success Rates and Fertility Outcomes
One of the primary goals of hysteroscopic adhesiolysis is to restore normal menstrual function and improve fertility outcomes for women with Asherman’s Syndrome.
Restoration of menstrual function
Studies have shown that hysteroscopic adhesiolysis can significantly improve menstrual regularity and reduce menstrual pain in women with Asherman’s Syndrome. By removing adhesions and restoring the normal uterine cavity, menstrual flow is able to pass freely, leading to improved menstrual function.
Improvement in pregnancy rates
Hysteroscopic adhesiolysis has also demonstrated positive effects on fertility outcomes. By removing the adhesions and creating a favourable environment for embryo implantation, the procedure can enhance the chances of successful conception and pregnancy. However, the success rates may vary depending on the extent and severity of the adhesions, as well as other individual factors.
Comparing Hysteroscopic Adhesiolysis with Alternative Treatments
Hysteroscopic adhesiolysis vs transcervical resection of adhesions
Transcervical resection of adhesions (TCRA) is another surgical technique used to treat Asherman’s Syndrome. While both hysteroscopic adhesiolysis and TCRA aim to remove intrauterine adhesions, they differ in the approach and instruments used. Hysteroscopic adhesiolysis allows for more precise visualisation and dissection of adhesions, making it preferable for complex cases. TCRA, on the other hand, involves the use of an electrosurgical device to cut or vaporise adhesions and may be more suitable for less severe cases.
Hysteroscopic adhesiolysis vs medical management
In some cases, hormonal therapy alone may be considered as a treatment option for Asherman’s Syndrome. However, while hormonal therapy can promote endometrial growth, it may not be sufficient for significant adhesions. Hysteroscopic adhesiolysis offers a more direct and targeted approach to remove adhesions and restore the uterine cavity, making it a more effective treatment option for moderate to severe cases.
Future Directions and Research
As medical technology continues to advance, there are ongoing efforts to further improve hysteroscopic adhesiolysis and its outcomes.
Innovations in hysteroscopic techniques
Researchers are exploring innovative techniques and instruments to enhance the precision and effectiveness of hysteroscopic adhesiolysis. This includes the development of advanced imaging technologies, such as three-dimensional hysteroscopy, which provides a more detailed visualisation of the uterine cavity.
Improving outcomes and patient satisfaction
Efforts are also going on to optimise postoperative care and follow-up protocols to improve patient outcomes and satisfaction. It includes personalised treatment plans tailored to each patient’s specific needs, additionally, comprehensive counselling and support throughout the recovery process.
Conclusion
Hysteroscopic adhesiolysis is a minimally invasive and effective treatment option for women suffering from Asherman’s Syndrome. By removing intrauterine adhesions, this procedure can restore menstrual function, improve fertility outcomes, and enhance the overall quality of life for affected women. With ongoing advancements in hysteroscopic techniques and postoperative care, the future looks promising for individuals diagnosed with Asherman’s Syndrome.
Frequently Asked Questions (FAQs)
- Q: Is hysteroscopic adhesiolysis a painful procedure? A: Hysteroscopic adhesiolysis is performed under anaesthesia, ensuring that patients do not experience pain during the procedure. Some mild cramping and discomfort may be experienced in the days following the surgery.
- Q: How long does the recovery process take after hysteroscopic adhesiolysis? A: The recovery time can vary from patient to patient. Generally, it takes a few days to a few weeks for the uterus to heal completely. Follow-up visits with your healthcare provider will be scheduled to monitor your progress.
- Q: Can hysteroscopic adhesiolysis improve my chances of getting pregnant? A: Yes, hysteroscopic adhesiolysis has been shown to improve fertility outcomes in women with Asherman’s Syndrome. By removing adhesions and restoring the normal uterine cavity, the chances of successful conception and pregnancy can be significantly increased.
- Q: Are there any risks or complications associated with hysteroscopic adhesiolysis? A: While hysteroscopic adhesiolysis is generally safe, there are potential risks, such as infection, bleeding, injury to the uterus or other pelvic structures, and anaesthesia-related complications. However, serious complications are rare.
- Q: Can Asherman’s Syndrome recur after hysteroscopic adhesiolysis? A: In some cases, Asherman’s Syndrome can recur after hysteroscopic adhesiolysis. However, with proper postoperative care and monitoring, the risking of recurrence can be minimised. Regular follow-up visits are crucial to evaluate the long-term success of the procedure.