Additional treatments we offer.
Preimplantation genetic diagnosis (PGD) \ Array Comparative Genomic Hybridisation (aCGH)
Handyside et al; (1992) first reported the use of PGD to detect genetically abnormal embryos before intrauterine transfer. PGD since then has undergone marked development and is becoming widely acceptable by the society. However, most studies showed PGD does not improve live birth rates per cycle especially in patients with advanced maternal age where cases of embryo aneuploidy are common.
By analysing genetic composition of cells biopsied from embryos PGD allows couples with high risk of having genetically disordered offspring to have a healthy child. Thus, PGD no doubt by preventing the selection of chromosomally abnormal embryos in IVF treatment cycles has recorded significant success in the improvement of pregnancy outcomes. PGD is clearly useful to screen, diagnose and prevent transmission of genetic diseases to offsprings. Its use has extended to include HLA tissue-typing – ‘saviour sibling‘ – Fanconi’s anaemia, and of course sex selection, screening for sickle cell trait.
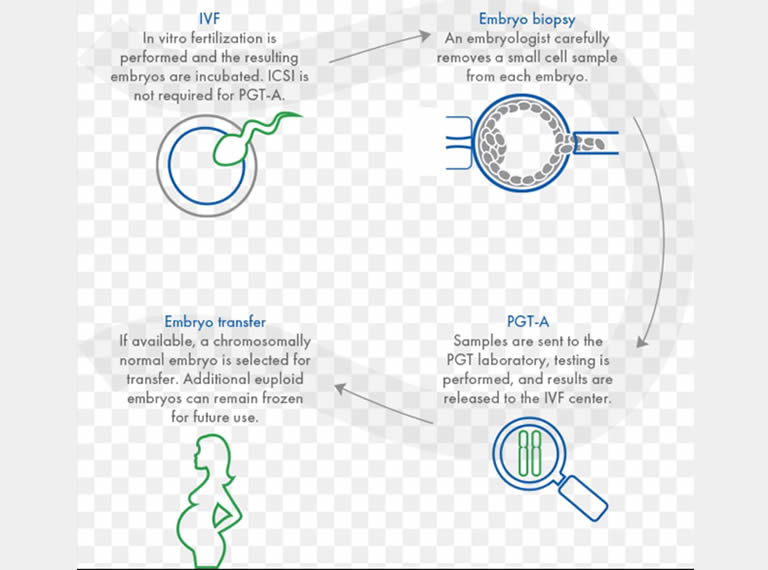
Cellular materials for PGD studies are obtained from either blastomeres from a day 3 embryo, trophectoderm from the blastocyst at day 5 or biopsies of the oocyte’s first and second polar bodies. Genetic tests can be done for single gene defects using polymerase chain reaction (PCR) analysis and for chromosomal anomalies using fluorescence in situ hybridization (FISH) analysis. For embryo selection in IVF a number of new genetic diagnostic techniques are available for example polar body array comparative genomic hybridization, whole genome amplification, quantitative PCR and SNP arrays.
Procedural and technical issues, increasing cost overlay on IVF and placental mosaicism are major drawbacks associated with PGD. Societal, religious and ethical concerns, dilemmas, and morality of PGD particularly on eugenic implications, sex selection for social reasons, possibility to make “designer babies” and risks of aberrations in the genetic imprinting processes vis a vis absence of significant improvement in live birth rates and the ever increasing cost of new genetic technologies are some of the drawbacks associated with the PGD processes. For these reasons PGD is not permitted in some countries like Germany and highly regulated by the government in the UK. In most developing countries like Nigeria the technique is most unavailable and where available it is unregulated.
Despite early concerns about unwittingly over-manipulating the embryo and the potential damage to biopsied embryo either at the cleavage or blastocyst stages; and also its potential use for eugenic purposes, PGD have found wider applications in reproductive medicine beyond the prevention of inheritable disease associated with aneuploidies such as Trisomies 13, 18 and 21 or autosomal (such as cystic fibrosis, sickle cell diseases, myotonic dystrophy) or X-linked chromosomal abnormalities such as (Duchenne muscular dystrophy, fragile-X syndrome) to name but a few (Braude et al., 2003). Other successful applications of PGD reported include cases of implantation failures, autosomal/X-linked diseases; chromosomal structural aberrations; recurrent idiopathic miscarriages and in stem cell research and for therapeutic uses.
Opening Hours
Saturday: 10:00am-4:00pm
Sunday: 10:00am-1:00pm
