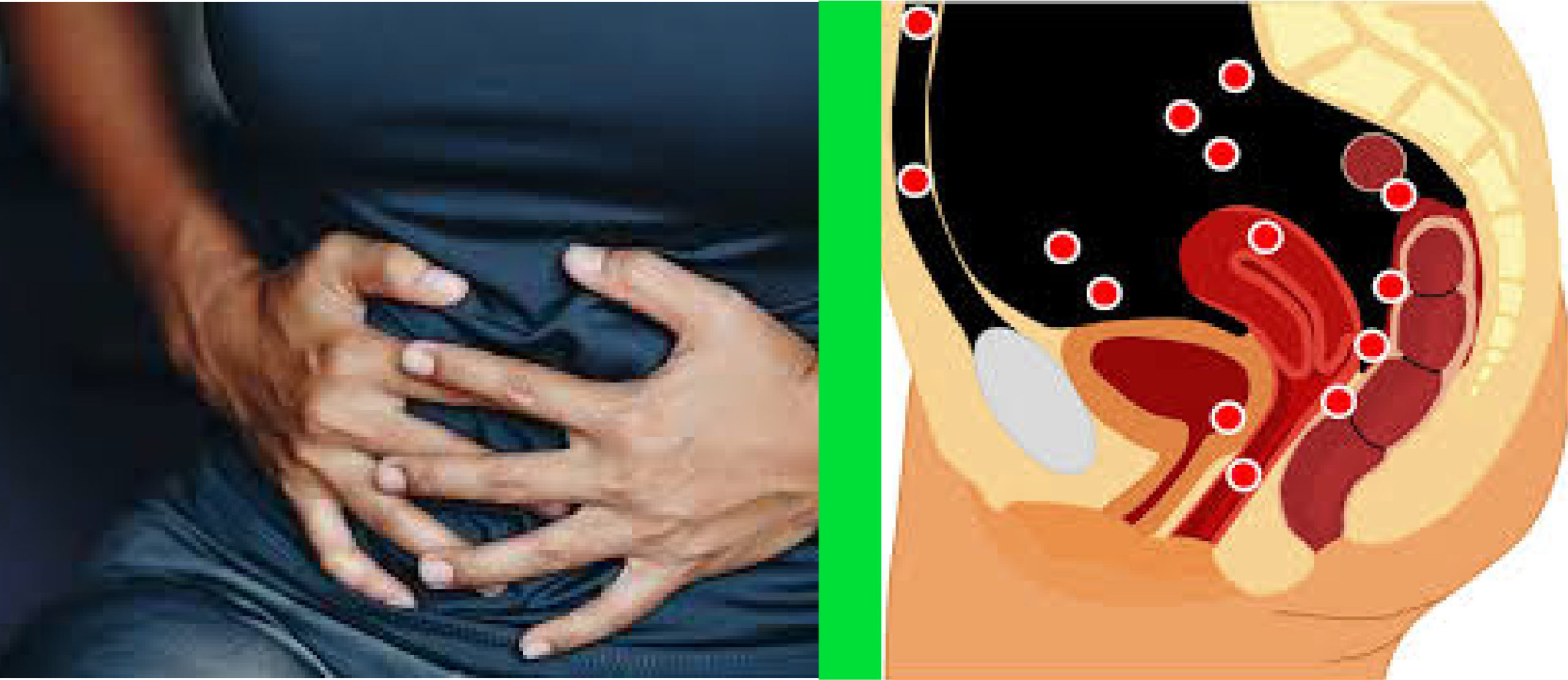
Endometriosis refers to the presence of endometrial (womb) tissues and glands outside the uterus, including the chest, abdominal or pelvic cavities.
It affects approximately 5% of fertile women and 20-40% of infertile women.
Pathogenesis of infertility in mild endometriosis is not yet clear but there are strong associations with increased miscarriage, peritoneal inflammation, immunologic/cytotoxic factors, and unruptured luteinised follicles. However, pathophysiological associations of endometriosis and infertility involve abdominal/ pelvic adhesions, tubal damage and/or ovarian destructions, ovulatory dysfunction, gamete and embryo cytotoxicity, immune system dysfunction and poor endometrial receptivity.
Symptoms: Presenting symptoms include abdominal pain of varying severity, often unrelated to the stage or extent of endometriosis. Furthermore, painful sexual intercourse (dyspareunia), painful defecation (dyschexia), severe menstrual pain (dysmenorrhoea), and association with poor quality of life are not uncommon.
Diagnosis: Abdominal and pelvic palpation may be tender usually with no palpable masses. Pelvic ultrasound scan to detect ovarian cyst (endometrioma) and other pathologies. Laparoscopy will reveal endometriotic spots and nodules in the pelvis especially on the ovaries, uterosacral ligaments and the pouch of Douglas; endometrioma and adhesions of
Treatment Modalities
Drug treatment for symptomatic control. For pain simple analgesia, nonsteroidal anti-inflammatory (NSAIDs) or opiods in women with pain associated with endometriosis and for menorrhagia are effective.
Hormonal preparations including combined oral contraceptive pills, progestagens and gonadotrophin releasing hormone analogues. Prolonged or extended uses of combined oral contraceptive pills or other hormonal preparations can compromise fertility, prevents ovulation and menstruation.
There is some evidence that Mirena IUS relieves pain and reduce menorrhagia in patients with endometriosis. Gonadotrophin-releasing hormone analogues (GnRHa) relieve symptoms of endometriosis, however, add back oestrogen should be added for prolonged usage (usually not advisable more than 12 months at a time) to prevent osteopenia/osteoporosis. Treating women for three to six months with GnRH agonists before IVF or ICSI increases the odds of clinical pregnancy four-fold.
Surgery (predominantly key-hole; laparoscopy) have significant FERTILITY BENEFITS over medical treatment of endometriosis in infertile patients.
In summary, moderate and severe endometriosis causes significant decrease in fertility especially with severe pelvic adhesions involving the ovaries and the fallopian tubes. Surgical interventions (ovarian cyst (endometrioma) excisions, adhesiolysis, electro-ablation of endometriotic spots, and tubal surgery) compared to medical treatments improve fertility in patients with pelvic endometriosis. As mentioned above treating women for three to six months after surgery with GnRH agonists before IVF or ICSI increases the odds of clinical pregnancy four-fold.
Laparoscopic excision of endometrioma of more than 4cm diameter is associated with decreased recurrence, control of symptoms, achievement of a spontaneous and/or IVF pregnancies compared to draining and coagulation.
Do you have ENDOMETRIOSIS or any of its associated problems?
Is it painful menstruation, painful sex, associated poor quality of life or infertility issues; we will work with you to find clinically effective treatment regimen that is evidence based.
If suffering from endometriosis and its associated symptoms; why keep it to yourself!
We are available to help and work with you to achieve effective solutions.
Please call us, send a text, or email us for consultant specialist appointments and treatments.
Opening Hours
Saturday: 10:00am-4:00pm
Sunday: 10:00am-1:00pm
