Disadvantages of the HSG Test
Disadvantages of the HSG Test: What to Consider Before You Proceed
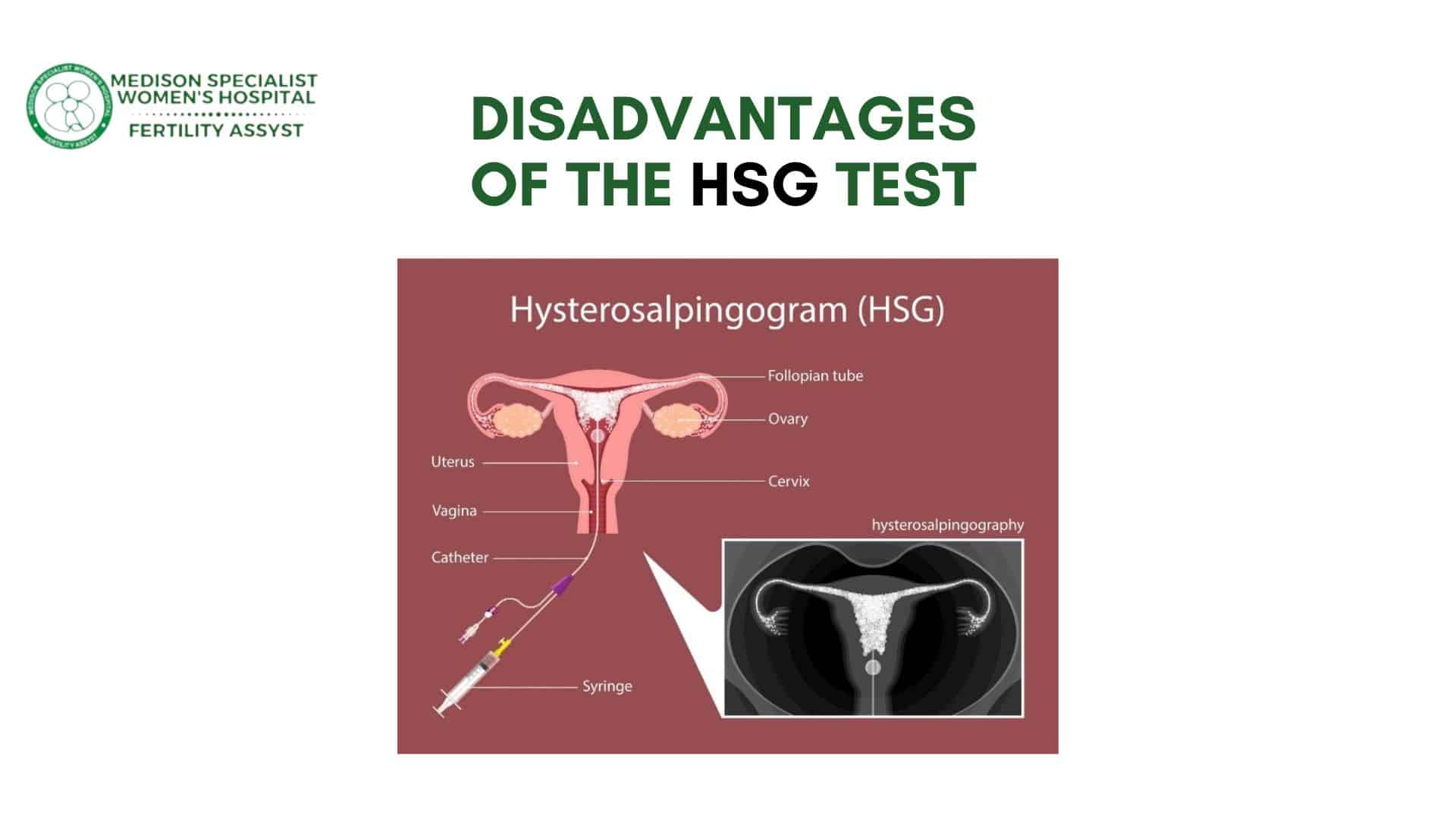
While the Hysterosalpingography (HSG) test is a valuable tool in fertility investigations, helping to identify blockages in the fallopian tubes and uterine abnormalities, it’s important to be aware of its potential disadvantages. Although this diagnostic procedure offers several benefits, including quick results and valuable information to guide fertility treatment (as discussed in our previous article on the advantages of the HSG test), some drawbacks should be considered before the procedure. In this article, we’ll outline the possible disadvantages of the HSG test, helping you make a more informed decision about your fertility journey.
Disadvantages of the HSG Test
1. Discomfort and Pain
One of the most common disadvantages of the HSG test is the potential for discomfort or pain during the procedure. While many women report only mild cramping, others experience more intense discomfort. The pain typically occurs when the contrast dye is injected into the uterus and fallopian tubes, as the uterus and cervix can be sensitive during this time.
Although the discomfort usually subsides within a few minutes, some women may find the procedure unpleasant or even difficult to tolerate. If you are particularly sensitive to pain or have a history of painful periods or uterine conditions, it’s important to discuss your concerns with your doctor beforehand so that they can help manage your experience.
2. Risk of Infection
Although the risk of infection after an HSG test is relatively low, it is still a potential concern. Since the procedure involves inserting a catheter into the uterus and injecting contrast dye, there is a small risk of introducing bacteria into the reproductive system. This can lead to an infection, particularly if the procedure is not performed in a sterile environment or if the patient has any pre-existing conditions that affect the reproductive organs.
To minimize this risk, your doctor will typically prescribe antibiotics before and/or after the procedure. It’s also essential to follow any post-procedure instructions carefully, such as avoiding sexual intercourse for a few days or monitoring for any unusual symptoms.
3. Not 100% Accurate
While the HSG test provides valuable insights into the health of the uterus and fallopian tubes, it is not foolproof. Some issues, such as very small blockages or subtle abnormalities, may not be visible on an X-ray, which could result in a false negative. In some cases, the test may suggest that a tube is blocked when, in reality, it is not. On the other hand, some women may have a clear HSG result but still face fertility issues due to factors that the test cannot detect, such as egg quality, male infertility, or hormonal imbalances.
As a result, while an HSG test is a helpful tool, it may not provide the complete picture. This is why fertility specialists often recommend combining it with other diagnostic tests, such as blood work or ultrasound, to obtain a more comprehensive understanding of your reproductive health.
4. Radiation Exposure
The HSG test involves X-ray imaging, meaning there is some radiation exposure level. However, the amount of radiation used in an HSG test is generally considered low and unlikely to cause harm, especially when the procedure is performed properly.
Nevertheless, if you are pregnant or may be pregnant, the procedure should be avoided. Even low levels of radiation can pose risks to a developing fetus, particularly during the early stages of pregnancy. Women undergoing an HSG test are usually advised to take a pregnancy test before the procedure to rule out any possibility of pregnancy.
5. Timing Limitations
The timing of the HSG test is crucial. It is typically recommended to perform the test during the first half of the menstrual cycle, after menstruation but before ovulation. This is because performing the test during or after ovulation can increase the risk of infection or interfere with the test’s accuracy.
This timing restriction can sometimes be inconvenient for women with irregular cycles or for those who are trying to conceive quickly. Additionally, scheduling the test during the appropriate window may cause delays in the fertility treatment process.
6. Potential for Emotional Stress
For some women, the HSG test can be emotionally stressful. The procedure involves exposing your reproductive health to scrutiny, and the anticipation of the test results can add to the emotional burden of infertility. Some women also feel anxious about the potential for pain or discomfort during the test, while others may feel nervous about what the test may reveal.
While the test provides valuable information that can help guide treatment, the emotional strain of undergoing a fertility investigation can be overwhelming. It’s important to have a support system in place, whether through friends, family, or fertility counseling, to help you manage any feelings of stress or anxiety that may arise.
7. Limited to Specific Fertility Issues
The HSG test is focused primarily on examining the structure of the uterus and fallopian tubes. While it can provide information on blockages, abnormalities, and certain other issues, it does not assess egg quality, sperm health, or other factors that could affect fertility. Therefore, if the HSG test comes back normal, but you are still having trouble conceiving, it may indicate that other factors are at play, and further tests may be needed.
For example, conditions like Polycystic Ovary Syndrome (PCOS), endometriosis, or low sperm count cannot be diagnosed through an HSG test. In these cases, additional testing, such as blood tests, semen analysis, or laparoscopy, may be required.
Should You Consider the HSG Test?
While the HSG test can provide valuable information about fertility health, it’s important to consider both the advantages and disadvantages before proceeding. Potential discomfort, a small risk of infection, and the limited scope of the test may be drawbacks for some individuals. However, the test is generally safe, minimally invasive, and offers essential insights into reproductive health.
If you are struggling with infertility and are considering an HSG test, it’s a good idea to consult with your fertility specialist at The Medison Hospital. Your doctor will be able to explain the test in more detail, help you weigh the pros and cons, and determine whether it is the right step in your fertility investigation.
Conclusion
The HSG test can be a valuable tool in diagnosing fertility issues, particularly when it comes to identifying blockages in the fallopian tubes and uterine abnormalities. However, like any medical procedure, it has its potential drawbacks, including discomfort, a small risk of infection, and limitations in detecting other fertility issues.
Ultimately, it’s important to thoroughly discuss with your doctor whether an HSG test is appropriate for your situation. Your fertility specialist can help guide you through the process and provide the necessary support to help you achieve your reproductive goals.
For more information or to schedule an appointment with one of our fertility specialists, visit The Medison Hospital Fertility Services or call us at +234 816 906 0064.